Call Routing Analytics for Medical Practices
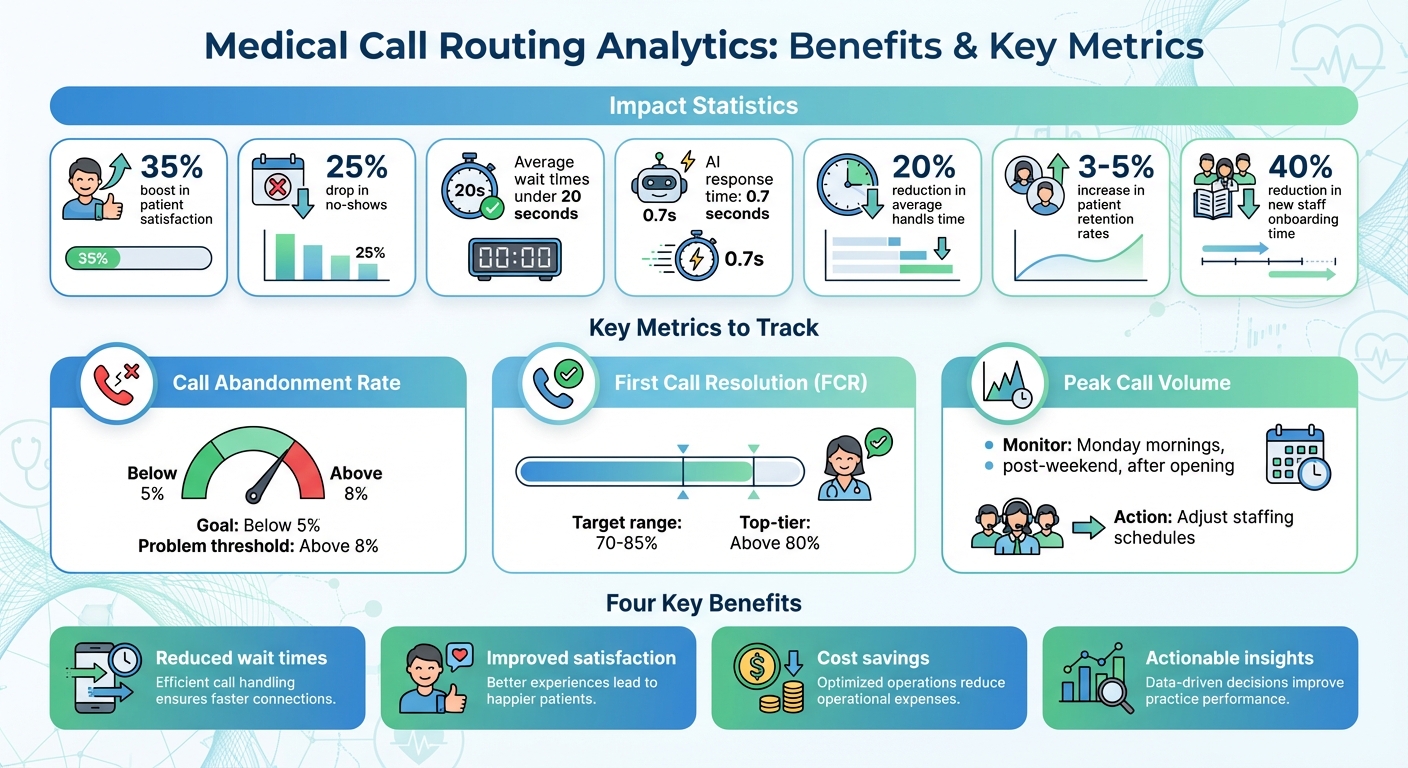
Call routing analytics helps medical practices manage patient calls more effectively by tracking every step from the first ring to resolution. It reduces wait times, prioritizes urgent concerns, and connects patients to the right department on the first attempt. Practices using these systems report a 35% boost in patient satisfaction and a 25% drop in no-shows, with average wait times under 20 seconds.
This tool also lightens staff workloads with features like AI-powered solutions that handle calls 24/7, respond within 0.7 seconds, and ensure HIPAA compliance. Key metrics like call abandonment rate, first call resolution, and peak call volume help identify bottlenecks, improve efficiency, and enhance patient experiences. By integrating with existing systems like EHRs or CRMs, practices can ensure seamless operations while reducing costs.
Key Benefits:
- Reduced wait times: Patients are routed quickly to the right staff member.
- Improved satisfaction: Faster resolutions and fewer transfers.
- Cost savings: AI tools reduce staffing needs and optimize resources.
- Actionable insights: Metrics reveal issues like high abandonment rates or inefficient call flows.
To implement, start by auditing your phone system, setting clear goals, and selecting HIPAA-compliant platforms with intelligent routing and reporting tools. Regularly analyze data to refine processes, adjust staffing, and test new strategies for better performance.
Call Routing Analytics Benefits and Key Metrics for Medical Practices
Benefits of Call Routing Analytics in Healthcare
Reduced Patient Wait Times
Call routing analytics in healthcare leverages real-time data to efficiently connect patients to the right department or staff member. Instead of being shuffled between extensions or stuck in the wrong queue, patients are directed to the correct representative on the first attempt. Urgent medical concerns are prioritized over routine administrative calls, significantly cutting down hold times.
For example, one healthcare provider saw a 20% drop in average handle time after adopting analytics-based routing. These tools also help identify bottlenecks in call flows, like overly complex IVR menus, enabling providers to streamline their phone systems and reduce delays. This level of efficiency not only improves patient experiences but also reduces operational costs.
Improved Patient Satisfaction Scores
Research from Press Ganey highlights a direct link between call center performance and patient satisfaction. Optimized call centers can increase patient retention rates by 3–5%. When patients quickly reach a knowledgeable agent who resolves their concerns without unnecessary transfers, their overall experience improves. Virtual contact centers with intelligent routing further enhance trust by ensuring prompt and consistent responses across all locations . This boost in satisfaction doesn’t just improve relationships - it can also lead to measurable financial benefits for healthcare providers.
Cost Savings for Medical Practices
AI-powered call routing analytics eliminates the need for manual triaging, freeing up clinical staff to focus on patient care rather than phone calls. For instance, one healthcare organization reduced new call center staff onboarding time by 40% by using analytics to unify call flow management. Additionally, call tracking analytics can pinpoint which marketing channels drive real appointments, helping practices fine-tune their advertising budgets . Solutions like Answering Agent can handle unlimited calls, removing the need for fixed staffing costs - a game-changer for smaller practices with limited budgets .
Analyze, Track and Improve Calls with Call Intelligence | Weave Walkthroughs
Metrics to Track for Call Routing Success
Metrics turn call routing into a science rather than a guessing game. For medical practices, having hard data is critical to ensure patients are connected quickly, their issues are resolved efficiently, and call traffic patterns are predictable. These insights reveal where your phone system shines and where it might be frustrating patients. In short, these metrics lay the groundwork for smarter, more efficient call routing.
Call Abandonment Rate
Call Abandonment Rate reflects the percentage of calls where patients hang up before reaching an agent. To calculate it, divide the number of abandoned calls by the total incoming calls, then multiply by 100. In healthcare, keeping this rate below 5% is the goal, while rates above 8% indicate serious problems like understaffing or ineffective routing systems.
When abandonment rates climb, it can lead to missed appointments and unhappy patients. A well-designed routing system, which connects callers to available agents in real time, can help minimize wait times and keep patients from giving up.
First Call Resolution (FCR)
First Call Resolution (FCR) measures the percentage of calls resolved during the first interaction. For healthcare practices, a solid FCR rate falls between 70% and 85%, with top-tier systems exceeding 80%. If patients are repeatedly transferred - like being bounced around for a billing inquiry - that’s a sign of poor FCR and operational inefficiency.
Routing calls based on patient history and directing them to specialists improves FCR and shortens handle times. For instance, sending billing questions directly to billing experts rather than the general front desk can make a big difference. Some healthcare providers using tailored call flows have even reduced their Average Handle Time by 20%, leading to quicker resolutions for patients and lower costs for the practice.
Peak Call Volume Analysis
Peak Call Volume Analysis pinpoints when your phones are busiest - often Monday mornings, right after opening, or following weekends. Understanding these trends allows practices to adjust staffing schedules to handle the rush, reducing wait times and lowering abandonment rates. These insights are key to fine-tuning call routing strategies for maximum efficiency.
sbb-itb-abfc69c
How to Implement Call Routing Analytics in Medical Practices
To make the most of call routing analytics in a medical setting, start by auditing your phone system. Take a close look at how calls are handled, identify common patient inquiries, and note peak call times. Then, set clear goals like reducing wait times, minimizing abandoned calls, and improving first-call resolution rates. Select a HIPAA-compliant VoIP or cloud-based contact center platform that offers intelligent routing, IVR menus, and detailed reporting features. These should include metrics like call volume, handle time, abandonment rates, and queue statistics. Adding call tracking can help you monitor source numbers, outcomes, and trends, especially across multiple locations or marketing campaigns.
For practices requiring 24/7 coverage, consider integrating an AI-powered answering service to handle calls around the clock. Link your phone system with your EHR, EMR, or CRM to automatically log caller information and call outcomes. This ensures your staff has all the necessary context before answering a call.
Below, we’ll explore how to configure routing rules, maintain compliance, and create tailored scripts.
Setting Up Intelligent Call Routing Rules
Organize incoming calls into priority levels: emergencies (redirected to 911 or an emergency line), urgent clinical issues (e.g., same-day triage, medication reactions, worsening symptoms), and routine requests (e.g., scheduling, prescription refills, billing inquiries). Configure your IVR to prioritize emergency and urgent calls by placing them at the top of the queue or directing them to a specialized triage team. Routine calls can be routed to standard queues or self-service options. Use caller attributes like patient type (new or existing), language preference, provider, or location to match calls with the right staff member.
Keep IVR menus simple and easy to navigate. Aim for 4–6 main options with clear, plain-language descriptions. Always include an option to speak to a live representative during business hours. Each IVR option should correspond to a specific call type in your analytics system, such as "New patient appointment" or "Billing question", allowing you to track key metrics like wait times and abandonment rates for each category. Avoid generic "other" categories; instead, base your menu on real-world call patterns gathered over a couple of weeks through call monitoring and staff input. Test the system with a small group of patients or front-desk staff to ensure it’s intuitive and minimizes unnecessary transfers.
Once your routing rules are in place, turn your attention to compliance.
Ensuring HIPAA Compliance
Any vendor supporting your call routing, analytics, or AI answering services must sign a Business Associate Agreement (BAA) and meet HIPAA’s strict requirements for administrative, physical, and technical safeguards. Since call recordings, transcripts, and analytics logs often contain protected health information (PHI), ensure that data is encrypted both during transmission and at rest. Access should be limited to authorized personnel, with role-based permissions and clear audit trails in place. For AI services, restrict PHI to only what’s operationally necessary and use features like automatic redaction of personally identifiable information (PII) in transcripts to reduce risks.
Set clear policies for how long call data will be retained, who can access it for quality reviews, and how patients will be informed about call recording or automated services. Regularly assess your system’s security through vendor reviews and audits, checking for factors like data center locations, incident response plans, and subcontractor management. This ensures your compliance efforts keep pace with any updates to your routing and analytics systems.
After addressing compliance, focus on developing scripts tailored to medical scenarios.
Customizing Scripts for Medical Scenarios
Create call scripts that function as decision trees, capturing only the necessary clinical and operational information while keeping the conversation natural. Develop specific flows for common situations like scheduling new patient appointments, arranging follow-up visits, handling basic symptom intake, or processing medication refill requests. Standardize appointment booking scripts to include essential details and ensure consistent logic for matching patients with providers. Sending confirmation texts after booking can also help reduce no-shows.
For symptom intake, whether handled by non-clinical staff or AI, gather structured information such as onset, severity, and any red-flag symptoms. Set clear guidelines on when to escalate to a nurse or advise the patient to seek emergency care. Include compliance elements like identity verification, consent notices, and disclaimers in clear, plain U.S. English. Test these scripts with diverse patient groups to ensure they’re easily understood.
Once implemented, use analytics to evaluate script performance. Track metrics like time spent on each script step, escalation rates, and error occurrences. Use this data to refine both human and AI-driven scripts over time. Structured call flows not only improve accuracy but can also cut onboarding time for new hires by up to 40%, thanks to consistent guidance.
Analyzing and Optimizing Call Routing Data
Once your call routing system is live, the next step is to dig into the data to make it better. Your analytics dashboard holds the answers to key questions: Why are patients abandoning calls? When are your staff overwhelmed? Are your routing rules doing what they’re supposed to? The aim is to fine-tune your system using important performance metrics.
Start by reviewing weekly metrics like Average Handle Time (AHT), call abandonment rates, and first call resolution. Compare these figures to your initial launch data. Break down the results by call type, time of day, and queue. For example, healthcare providers who analyzed their call flows and fixed inefficiencies saw a 20% drop in AHT, which freed up staff time and improved patient access.
Take it a step further by linking phone metrics to patient outcomes and business results. For instance, track how many calls lead to booked appointments and measure no-show rates based on confirmation practices. According to research from the Advisory Board, healthcare organizations with well-optimized call centers experienced a 3–5% boost in patient retention, which directly supports revenue. Showing that reducing abandoned calls translates to more appointments makes a strong case for ongoing improvements.
Your analytics platform’s real-time dashboards are also a powerful tool. Use them to keep tabs on live call volume, queue lengths, and agent availability throughout the day. For practices with multiple locations, centralized visibility can make a big difference by routing overflow calls from one office to available staff at another. Set up alerts to notify you when wait times or abandonment rates exceed acceptable limits, so you can act quickly.
But don’t just rely on numbers. AI-powered, HIPAA-compliant transcription tools can analyze call recordings to identify keywords like "pain", "urgent", or "billing issue." These insights can help classify call intent and flag potential quality issues. When paired with proper safeguards for PII and HIPAA compliance, this qualitative data adds another layer of understanding to why certain routing paths may not be working.
By continuously reviewing and analyzing this data, you’ll be able to zero in on specific call flow issues.
Identifying Bottlenecks in Call Flows
To identify where things go wrong, map the full call journey - from the moment a patient dials to when their issue is resolved or they hang up. Include every IVR menu, queue, transfer, and hold period. Overlay this map with your metrics to pinpoint problem areas, like delays or high abandonment rates.
Common bottlenecks often show up as queues with long wait times, unclear IVR menus, or areas where patients frequently hang up. Listening to call recordings or reviewing AI transcriptions can shed light on why patients give up - whether it’s confusing menu options, extended hold times, or difficulty reaching a live agent. Simplifying the call flow using the "Rule of ONE" (one clear primary path per scenario) can speed up resolutions. One healthcare provider, for instance, streamlined their system and cut staff onboarding time by 40%, making it easier to scale and maintain consistency.
Once you’ve identified these bottlenecks, you can use the insights to improve staffing and scheduling.
Using Data for Staffing and Scheduling
Historical call data is a goldmine for predicting staffing needs. Look at call volume trends by hour, day, and season to identify peak times - like Monday mornings, post-lunch periods, or flu season surges. Use this information to align your staffing schedules with demand.
You can also track the reasons behind calls to fine-tune scheduling even further. For example, if certain types of calls spike during specific times, ensure that staff with the right expertise are available. Pairing call analytics with appointment data can help you adjust hours and staffing levels for better efficiency.
Once you’ve optimized staffing, consider experimenting with different routing strategies to improve performance even more.
A/B Testing Routing Strategies
Testing different routing strategies can reveal what works best for your patients. For instance, compare a direct-to-agent system with an IVR-based approach, or test skill-based routing (like a Spanish-speaking line or a pediatric specialist) against a general queue.
Split your calls between the current system and the new strategy. Then, measure key metrics like average speed of answer, abandonment rate, first call resolution, appointments booked, and patient satisfaction. Run these tests for two to four weeks to capture typical call patterns and avoid skewing results due to one-off events.
Don’t just focus on numbers - use AI transcription and sentiment analysis to gauge differences in patient language and tone between test groups. This can offer deeper insights into the overall experience.
Make small adjustments and re-test regularly, especially when introducing new services, locations, or telehealth options. Always ensure that testing and analytics comply with HIPAA standards by using encryption, access controls, and proper PII redaction in any AI tools. This approach ensures your call routing system adapts to both patient needs and your practice’s capabilities.
Conclusion
Call routing analytics has become a must-have for U.S. medical practices. Every incoming call represents an opportunity - whether it's about patient care or revenue. Poorly managed routing can result in missed appointments, unhappy patients, and overwhelmed staff. On the other hand, healthcare organizations that streamline their call centers often see measurable improvements in patient retention and call handling efficiency.
Start by focusing on key areas like reducing call abandonment rates, resolving issues on the first call, and improving telehealth triage. Implement intelligent routing rules that consider factors such as call purpose, patient status, and staff expertise. Keep a close eye on critical metrics like abandonment rates, first-call resolution, peak call patterns, and response times using real-time dashboards. Make sure your system is HIPAA-compliant, featuring secure call recording, PII redaction, and proper Business Associate Agreements. Remember, optimization isn’t a one-and-done task - it’s an ongoing effort that keeps your practice efficient and patient-centered.
For even more impact, consider integrating call routing analytics with AI-powered tools like Answering Agent. These platforms operate 24/7, handle unlimited calls during high-volume periods, and even book appointments when your front desk team is unavailable. They ensure consistent patient interactions through customizable scripts and feed valuable data - such as call reasons, outcomes, and booking rates - back into your analytics. With HIPAA-compliant features and seamless integration with practice management systems, AI answering services make sure every patient inquiry is addressed while helping you maximize revenue opportunities.
Faster response times, clear communication, and data-driven staffing decisions don’t just enhance the patient experience - they also improve your practice’s financial performance. Practices that prioritize measuring their current performance, adopt compliant tools, and refine processes based on real call data can see noticeable improvements in just a few weeks. Every call should bring patients closer to the care they need while reinforcing your practice’s operational strength and financial health.
FAQs
How can call routing analytics help medical practices enhance patient satisfaction?
Call routing analytics play a key role in helping medical practices enhance patient satisfaction by simplifying the way calls are handled. These tools offer critical insights into call patterns, pinpoint areas where delays occur, and reveal ways to cut down on wait times.
When patients are quickly directed to the right team member and provided with accurate, tailored support, the entire experience becomes more seamless and efficient. This approach not only builds patient trust but also elevates the quality of care and service the practice delivers.
What key metrics should medical practices monitor to improve call routing efficiency?
To make call routing more effective, medical practices should keep an eye on key metrics like call volume, call abandonment rate, average wait time, call duration, call transfer rate, and patient satisfaction scores. These indicators shed light on how efficiently calls are being managed and highlight areas that might need attention.
It’s also important to monitor call outcomes, such as how many appointments are booked or issues are resolved during calls. This added layer of tracking can help refine patient interactions and streamline overall operations. By focusing on these data points, practices can cut down on wait times, enhance service quality, and create a better experience for patients.
How can medical practices stay HIPAA-compliant while using call routing analytics?
To ensure compliance with HIPAA regulations, medical practices must rely on secure platforms specifically designed to safeguard patient data and privacy. This involves a few critical measures: encrypting sensitive information, restricting access to only authorized individuals, and maintaining comprehensive audit logs to monitor system activity.
Equally important is staff training on HIPAA rules. Educating your team ensures everyone understands how to handle protected health information (PHI) appropriately. Additionally, selecting a platform with built-in protections for PHI not only shields your practice but also strengthens patient trust in your commitment to their privacy.
Related Blog Posts
Related Articles
How AI Enhances Patient Engagement in Telehealth Scheduling
AI scheduling cuts no-shows, shortens wait times, and boosts patient engagement with 24/7 personalized booking, predictive reminders, and waitlist automation.
How AI Handles High-Volume Appointment Calls
AI-driven phone agents answer every appointment call, sync with EHRs, and recover lost revenue while cutting staff workload.
Multilingual AI Telehealth: ROI for Medical Practices
Multilingual AI telehealth enhances patient care and reduces costs by overcoming language barriers, transforming healthcare practices financially and operationally.
